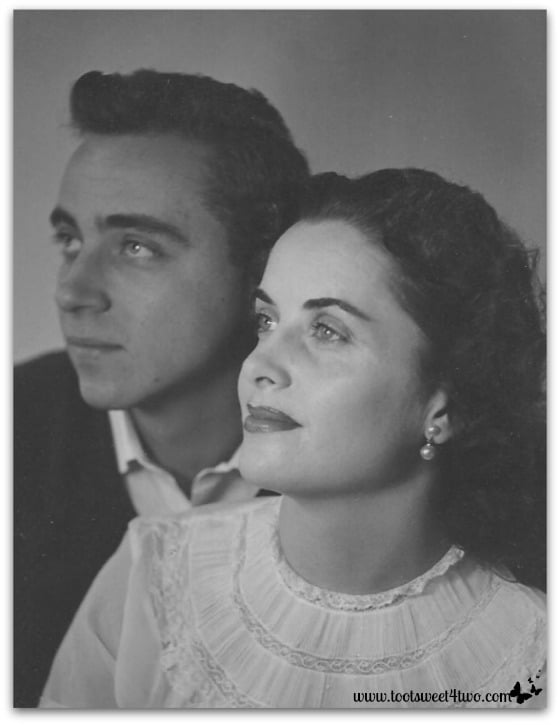
My parents, circa 1950
The Best of the Rest of Your Life…that’s what I want for my elders. I’ve just returned from spending several hours with my mother at her residential care facility. I meant to visit her on Friday. Then it was Saturday. Now it’s Sunday.
Somehow, the weekend just got away from me. And, I’m sitting at my computer writing this and crying.
Crying because I can’t fix it. I can’t fix a system that’s broken. I can’t make people simply do their jobs. Why can’t people simply do their jobs?
This is a tough post for me to write. I’m been mulling this one over in my mind for more than you year now…since the death of father in January 2013, under hospice care.
My father had severe heart disease. He knew he would die. Don’t we all know we are going to die? But, did he have to die when he did?
That’s the question that haunts. Because I feel, very strongly, that “the system”, that I, let him down.
More than 20 years ago, my parents had “the talk” with me. The talk about their end of life wishes. I was in my late thirties and as all children who have experienced “the talk” with their parents know, I didn’t want to have this talk. I pooh-poohed the seriousness of “the talk” and with a nonchalant wave of my hand dismissed “the talk” by telling them it was too early to have “the talk.”
But, out of respect for them, I listened intently as they shared their wishes.
And, as they’ve aged (suddenly it seems to have descended so quickly), because of “the talk”, I’ve had a clear understanding of what they wanted.
For more than 5 years now, our elder care journey has been fraught with one major health crisis after another. Each one has normally required an extended stay at a skilled nursing center, following hospitalization, until they were well enough to return to the assisted living facility, their home. While at the skilled nursing center, if they are there more than a month, this center has a meeting with the patient, the patient’s family and the heads of the different “disciplines” – the head of nursing, the head of physical therapy, the dietician, the head of occupational therapy, the social worker, etc. It was not unusual that 10 people would be in the room to discuss the patient’s progress.
Without fail, one of them (usually the social worker) would look straight at my parent and ask them their end of life wishes. Every single time – every. single. time. – my parent (both of them) would express that they wanted to live. In medical terminology, full code.
As a participant at these many meetings, plus because of “the talk”, I always knew, positively, my role in helping my parents as they aged.
And then in October 2012, the rules changed. My father was in the hospital recovering from his latest bout of congestive heart failure. I was not there; I was at work. A doctor asked him if he wanted to be intubated. My father said no.
Let me explain this a little better – the doctor came into my father’s room to talk to my father who was awake, alert and doing well, on his way toward discharge and home. In the hospital, whether in the emergency room or as a patient admitted into the hospital, doctors (at least in my experience) always ask elders their end of life wishes and during that conversation, ask the elder if they want to be intubated. Always, in the past, my father said yes.
So, my father did not need to be intubated at that very moment; the doctor was asking him this question during the course of the normal end of life questioning that my father had gone through many times before. This wasn’t a moment of crisis with my father refusing medical care.
But, my father’s “no” set wheels in motion that brought the hospice system into play. At no time during this process did my father sign a “do not resuscitate” order, which is part of the normal procedure in the hospice process. Someone, or multiple someone’s, did not do their job.
Within 3 months (January of 2013), he passed away. As he lay struggling to breathe, I asked that he be taken to the emergency room. The hospice nurse said, “you realize that this will negate hospice care?”
I said, “I don’t care; I want my father helped.”
She said, “but, he signed a Do Not Resuscitate order.”
“I’ve never seen a Do Not Resuscitate order. Show it to me.”
She went over to his file on the dresser and after rifling around in it for a few minutes said, “that’s odd; it isn’t here.”
And, I said, “that’s because he’s never signed one. He’s always told me he wants to live.”
The nurse, frustrated that I was now asking her to do something that was against the very nature of what she was trained to do, called the hospice office. After a brief conversation with the person on the other end, she handed the phone to me. I stepped out of the room, into the hallway to have this conversation.
The young man on the other end could not confirm that my father had signed a “do not resuscitate” order. And, they could not produce one; even an electronic version, because one didn’t exist.
In my anger, I hung up the phone and went back into my father’s room ready to do battle with the nurse and get my father to a hospital. But, it was too late and my father passed away…
If hearing is the last thing to go (as I’ve been told by hospice personnel), then the last thing my father heard was me telling the nurse to call an ambulance to take him to the hospital and her telling me that it would “negate hospice. He signed a ‘do not resuscitate’ order.” The system failed him. I failed him.
I’m sharing this now because “the system” is failing my mother. She’s been hospitalized recently and has returned to her assisted living facility. Plus, she was taken to ER this past Thursday, treated and released. In both instances upon her return home to her assisted living facility (so now going on almost a month), she requires a higher level of care. For almost a month now, I’ve asked this facility to provide her with that higher level of care (at more cost to my mother; so I’m not asking that it be free) and they have assured me that she is getting the needed additional care. A week ago, I had a two-hour, face-to-face meeting with the Assisted Living Director and her assistant and we had a detailed conversation about my expectations of my mother’s care.
However, each time I visit her, something just isn’t right and I call it to the attention of the care facility. I do this in a nice way. I’m not the type of person that “demands” things nor am I unpleasant. These aren’t nitpicking requests; they are requests to improve her “activities of daily living,” i.e., help with eating, help with toileting, help with cleanliness. I am thorough and very detailed in my expectations. And, I expect people to do their job.
Twice in the last week, I’ve had caregivers suggest to me that maybe it’s “time” to put my mother in hospice. I have, emphatically, said no. My mother does not have a life-threatening illness. She does not have a fatal illness. She is recovering from the flu. She has told me, even today, that she wants to live to be 100. My understanding of her wishes is clear.
So, imagine my surprise today when I found out that my mother was not on the medication she was prescribed upon her release from ER on Thursday. For 3 days, she has not received a medication that is critical to her recovery. Ordering the prescribed medication “slipped through the cracks.” Someone did not do their job.
By the way, this assisted living facility is a “nice” facility. My mother pays a substantial fee to live there. When deciding to move there two years ago, my mother visited 10 different facilities before choosing this one.
Don’t get me wrong – I have great admiration for people in the medical and caregiving fields. The majority of the doctors, nurses and caregivers that I have met and gotten to know throughout this journey have been extremely competent and exceeding kind. But, when the system fails, it fails shamefully, shockingly, appallingly. You see, when someone doesn’t do their job in the medical and caregiving fields, it can lead to serious illness and death.
This is my open letter to the caregiving community. Please, do your job. The lives of our elders and other loved ones are at stake. They need you when they are most vulnerable. Please don’t let them down. If it was your mother, what would you do?
My mother loved to garden. The following photos I share with her in mind. Some are the same photo, just cropped differently. Because I can’t decide. My aching heart has made me indecisive in choosing from the thousands of photos I’ve taken this past year. I chose 8 flowers photos for her and then couldn’t decide how to crop them.
This is me. Being indecisive. Because I can’t make it better. I want to make it better. Please make it better. Please do your job…








I love you, Mom…

Related Posts:
(other posts in The Eldercare Diaries)
My 100-year-old grandmother is at a facility and my mom found her sleeping in the bathroom the other day. It made her livid.
It’s a heartbreaking story and I fear we all will have to live it. My super strong, ambitious grandmother – is she getting the care she deserves?
You’re right, Tamara. It’s a heartbreaking struggle for all of us that are fortunate enough to have elder loved ones with us.
This is such a heartbreaking piece. My mother-in-law is starting to have some health troubles, so we’re just getting in to this minefield of medical care. There’s a lot to think about. (And I understand even more so in the US than here in the UK!)
Thanks, Rachel, for your words of support. I’m so sorry to learn about your mother-in-law. Elder care is often such a tough, emotional road to travel.
My father is coming close to the end and its hard to believe, sometimes I just don’t want to deal with it. I try to talk to my mom and she doesn’t want to deal with it either. I empathize with your situation and dealing with doctors. I am so sorry you had to go through that.
It’s so hard to watch loved ones struggle. I’m sorry, too, that it’s happening to you now. Thanks for your support.
I totally understand your frustration and fear. You are doing the very best for your mother and you did the same for your father. You have not let them down at all, they are so blessed to have you. In the end, your father knew he was loved and adored by you. That is what is important. I know how painful this is. I wish I could ease your pain but it is so personal. Know you and your mom are in my thoughts and prayers.
Thank you, Anna, for the wonderfully worded, thoughtful and loving comment. I appreciate your love and support.
Love you Carole! Sending you a BIG hug! Kathy
Thanks, Kathy, for being such a wonderful and supportive friend. I needed that BIG hug today!